Finishing treatment for lymphoma is a big deal! You have overcome challenges you may have never thought you would be faced with, and probably learned a lot about yourself and what is important to you.
However, finishing treatment can come with challenges of its own. You may experience mixed emotions as you begin to work out who you are after cancer – or worry about how long you may be in remission for, and how to still enjoy life.
This page will discuss what to expect when treatment ends, and tips on how to manage life as it is now.
What to expect after finishing treatment?
Adjusting to life after lymphoma treatment can be a difficult time for many people. While finishing treatment can be a relief, many people say they’ve had challenges in the weeks, months and even years after treatment is finished.
After months of hospital appointments and regular contact with your medical team, it can be very unsettling for some, to only be seen once every few months or so. How often you continue to see your oncologist or haematologist will depend on several factors which include the below.
- The subtype of your lymphoma and any genetic mutations you have.
- How your body responded to treatment and if you have any side-effects that need ongoing monitoring.
- How long ago you finished treatment.
- Whether you had or have an aggressive or indolent lymphoma.
- Scan and test results.
- Your individual needs.
What support is available?
Just because you won’t be seeing your oncologist or haematologist as often, does not mean you are on your own. There is lots of support still available to you, though it may come from different people.
General Practioner (GP)
If you haven’t already found a regular local doctor (GP), now is the time to do it. You will need a regular and trusted GP to support you through your treatment, co-ordinate your care and provide important follow-up care after you finish treatment.
GPs can help by prescribing some medicines and referring you to different specialists and health professionals. They can also put together a care plan so you have a guide for when and how to get the support you need in the year ahead. Care plans can be updated yearly. Talk to your doctor about these plans and how they can help in your individual circumstances.
Click on the heading below to learn more about these care plans.
Cancer is considered a chronic illness because it lasts longer than 3 months. A GP management plan allows you to access up to 5 allied health consults per year with no, or very little out of pocket cost to you. These can include physiotherapists, exercise physiologists, occupational therapists and more.
To learn more about what is covered by allied health, please see the below link.
Allied health professions – Allied Health Professions Australia (ahpa.com.au)
Everyone with cancer should have a mental health plan. They are also available to your family members and provide you with 10 visits or telehealth appointments with a psychologist. The plan also helps you and your GP discuss what your needs will be over the year, and make a plan to cope with the extra stressors related to adjusting to life after lymphoma, or any other concerns you have.
Find more information on what mental health care is available here Mental health care and Medicare – Medicare – Services Australia.
A survivorship care plan helps to coordinate the care you need after a cancer diagnosis. You may have one of these done before you finish treatment, but not always.
A survivorship plan is a great way to look at how you will manage after treatment ends, including managing side-effects, anxiety, fitness and overall wellbeing.
Lymphoma Care Nurses
Our Lymphoma Care Nurses are available Monday to Friday 9am to 4:30pm EST (Eastern States Time) to talk you through your concerns and offer advice. You can contact them by clicking the “Contact Us” button at the bottom of the screen.
Life coach
A life coach is someone who can help you set realistic goals and make a manageable plan to achieve them. They are not psychologists and cannot offer psychological support, but can help with motivation, organisation and planning as you adjust to life after lymphoma or treatment. To learn more about life coaching service see the link below.
Peer support
Having someone to talk to you who has gone through similar treatments can help. We have an online peer support group on Facebook as well as ongoing online or face to face to face support groups. To access these, please see the links below.
Survivorship or wellness centers
Many hospitals or doctors are connected to survivorship or wellness centres. Ask your haematologist what survivorship or wellness centres are available in your area. Some may need a referral which your GP can help you with.
These support centres often offer complimentary therapies, exercise and lifestyle classes (such as healthy cooking or mindfulness). They may also have emotional support such as peer support, counselling or life coaching services.
Treatment and side effects
Many side-effects of lymphoma treatments happen during treatment. However, in some cases side-effects may last for months or even years after treatments ends. Side-effects from intensive treatments such as the high dose chemotherapy used before a stem cell transplant are more likely to take longer to improve.
Late effects
In some cases, you may get late-effects from treatment that start months or even years after treatment ends. While many of these are rare, it is important to be aware of your risk so you can have the appropriate follow-up and screening tests and catch any new condition early for the best treatment options.
For more information on side effects and late effects of lymphoma treatments, click the link below.
When will you feel better?
Recovering from treatment takes time. Do not expect to be back to full strength or health straight away. For some people it can take months to recover from lingering side-effects. For some, you may never return to your full strength and energy levels as before you had lymphoma.
Learning your new limits and finding new ways of living will be important for you. However, just because life may now be different, does not mean you cannot look forward to good quality of life. Many people use this time to re-evaluate what is meaningful for them and begin to let go of extra stressors in life we often hold on to unnecessarily.
Things that can impact your recovery include:
- The subtype of lymphoma you had/have and how it impacted your body
- The treatment that you had
- The side-effects you had during treatment
- Your age, general fitness and activity levels
- Other medical or health conditions
- How you feel in yourself both mentally and emotionally.
Returning to work or school
If you plan to return to work, studies, it may not always go to plan. It is important to be realistic and give yourself time to recover. Click on the scroll boxes below for some tips on returning work or school.
Work
It's a good idea to talk to them before you return to work to start planning your transition back to work. If you do not have a HR department, speak with your manager about how they can help you return to work in a safe and supported way.
Scroll over the card to find some tips on returning to work
Tips for returning to work
Reduced hours, or alternative days.
Work from home options.
Social distancing while your immune system recovers.
Easy access to masks and hand sanitiser.
Avoiding substances that can cause infection such as animal waste, raw meats, infectious waste.
A quiet place to rest if you become too tired.
Occupational therapy to review your workspace and needs.
School
Scroll over the card to find some tips on returning to work
Tips for returning to school
Reduced homework.
Options to complete school work at home or through distance education
Socially distanced classroom.
Easy access to masks and hand sanitiser.
A quiet, safe place to rest if you become too tired.
Education for a classmates and school on lymphoma (invite Lymphoma Care Nurses to come and speak).
Extend due dates for assessments.
Fear of return (relapse)
 Although lymphoma often responds very well to treatment, some of you will be told that it is likely your lymphoma will relapse at some time. In some cases, your doctor may say that it may relapse but that there is no way to tell if, or when it will return. Even if you’ve been told you are cured and its unlikely to come back, you may find yourself worrying about it.
Although lymphoma often responds very well to treatment, some of you will be told that it is likely your lymphoma will relapse at some time. In some cases, your doctor may say that it may relapse but that there is no way to tell if, or when it will return. Even if you’ve been told you are cured and its unlikely to come back, you may find yourself worrying about it.
It is normal to worry about this a little. You have been through a lot, and you may feel that your body already failed you once, so you may have less trust in your body’s ability to keep you safe and well.
This can cause hyperawareness, where you notice EVERY change in your body and start to become too focused on what is happening, fearing it’s related to lymphoma. Some people find it affects their ability to enjoy life and make plans.
Awareness versus hyper-awareness
Having awareness of your risk of relapse is important because it helps you identify new symptoms and get medical advice early. However, hyperawareness results in uncontrolled worry and fear, and has a negative effect on your quality of life.
Finding the balance between being aware of your risk and enjoying life to its fullest can take time. Most people say, the longer they are in remission the easier it gets to live with the uncertainty. Reach out and get support when you need it, or if you want to talk to through what you are feeling, or what is happening in your body.
Get support
You can speak with your GP, our Lymphoma Care Nurses, a counsellor or psychologist. They can all help you work through your fears and develop strategies for living with the reality of life after lymphoma treatment, while still enjoying life.
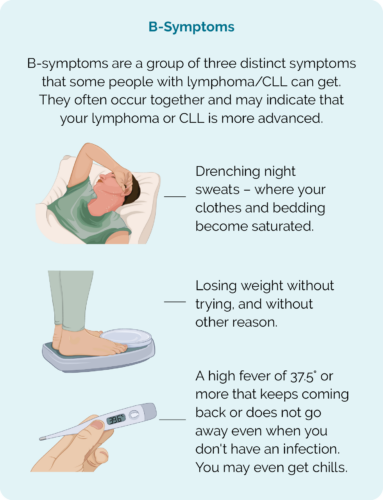
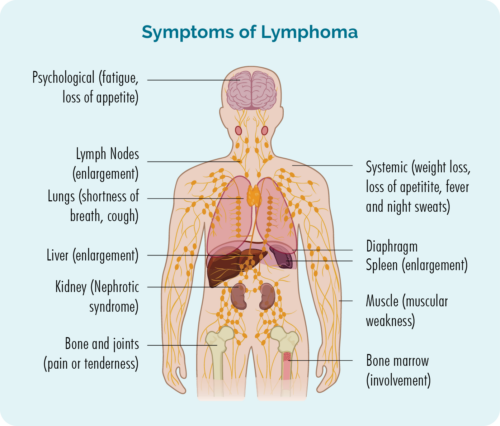
Report new symptoms to your doctor
As you learn what is now normal for you (after lymphoma treatment), it is important to report all new or ongoing symptoms to your doctor. It is important that your regular GP as well as your haematologist or oncologist are aware of any new or ongoing symptoms. They can then assess them and let you know if it is something that needs follow-up or not.
Ask your doctor:
- What should I look out for?
- What should I expect over the next few weeks/months?
- When should I contact you?
- When should I go to the emergency department or call an ambulance?
Emotional impact
It’s normal to have a mixture of feelings, and to have good and bad days. Some people describe getting cancer, having treatment and recovering, or learning to live lymphoma as a ‘rollercoaster ride’.
You may want to return quickly to your usual routines, or you may need time to rest after you finish treatment and process what your have been through. While some people prefer to ‘get on with it’, others say they want to learn to appreciate things more and prioritise what is important in their lives.
Whatever your approach is, your feelings and thoughts are valid, and nobody else can tell you what is right or wrong for you. However, if your emotions or thoughts are making it hard for you to enjoy life or make you fearful, reach out and get support. There are many support services and free counselling available to you.
Watch the video above for some tips on living with the emotional impacts of anxiety and uncertainty.
Expectations of others
You may have people in your life who think now treatment is over you should “just get on with life”, and not understand you still have physical and emotional limitations. Or on the contrary, you may have people in your life that try to hold you back because they are afraid of something happening to you, or of you “over doing it”.
Unless somebody has gone through treatment for cancer, there is no way for them to truly understand what you are going through, – and it would be unreasonable to expect them to. They may never truly understand the ongoing burden of side-effects or worry you live with.
Even people who have had cancer may not truly understand your experience, as cancer and its treatments affect people differently.
No matter how hard they try, there is no way for them to know exactly what you are going through, what you are struggling with, or what you are capable of.
Let people know
Often people try only to catch up with others when they are feeling well. Or, perhaps when you are asked how you are feeling, you gloss over the hard stuff and just say you’re doing fine, or ok.
If you’re not honest with people about how you are doing, how you’re feeling and what you’re struggling with, they will never be able to understand you may still need support – or know how they can help.
Be honest with the people closest to you. Let them know when you need support and that your experience with lymphoma is not yet over.
Some things you might like to ask for include:
- Cooking a meal you can keep in the freezer.
- Help with housework or shopping.
- Someone to sit and chat, or watch a game/movie, or enjoy a hobby together with.
- A shoulder to cry on.
- Picking up or dropping kids off at school or play dates.
- Going for a walk together.

What happens if my lymphoma relapses?
The first thing you need to know is that even many relapsed lymphomas can be successfully treated.
It is not uncommon for some lymphomas to relapse. Relapsed lymphoma can often be successfully treated, resulting in cure or another remission. The type of treatment you will be offered depends on several factors including:
- What subtype of lymphoma you have,
- How many lines of treatment you have had,
- How you responded to other treatments,
- How long you were in remission for,
- Any ongoing, or late-effects you may have from previous treatment,
- Your personal preference once you have all the information you need to make an informed choice.
To learn more about relapsed lymphoma, please see the link below.
Frequently asked questions (FAQs)
Hair usually starts to grow back within weeks of finishing treatment with chemotherapy. However, when it does grow back it may be very thin – a bit like a new babies. This first bit of hair may fall out again before growing back.
When your hair does come back, it may be a different colour or texture than it was before. It may be curlier, greyer or grey hair may have some colour back. After about 2 years, it may be more like the hair you had before treatment.
Hair normally grows about 15cm each year. That’s about half the length of an average ruler. So, 4 months after you finish treatment, you may have up to 4-5cm of hair on your head.
If you have radiotherapy, the hair on the patch of skin treated may not grow back. If it does, it may take years to start growing back, and still not grow back to the normal way it was before treatment.
For more information on hair loss, please click the link below.
How long it takes for your immune system to get back to normal depends on what type of treatment you had and the subtype of lymphoma you had/or have.
Neutrophils
Your neutrophils will usually return to normal within 2-4 weeks of finishing chemotherapy. However, some treatments such as monoclonal antibodies, radiotherapy or stem cell transplants may result in a slower recovery of, or late onset neutropenia.
If your neutrophils do not recover your haematologist or oncologist may offer you growth factors to stimulate your bone marrow to make more. You will need to continue to take precautions to avoid infection, and let your doctor know if you become unwell. Go to emergency immediately if you have a temperature of 38° or more. For more information on managing neutropenia click here.
Lymphocytes
B-cell lymphocytes make antibodies, but they need T-cells to help activate them to make the antibodies. Therefore, whether you had B or T-cell lymphoma you may have less antibodies after treatment.
Antibodies are an important part of our immune system, attaching to germs and diseased cells to attract more immune cells to come and eliminate the diseased or damaged cells. Most people will have a return of antibodies as your diseased lymphocytes (lymphoma cells) are destroyed and new, healthy lymphocytes take their place. However, a small number of you will have ongoing issues with low antibodies. This is called hypogammaglobulinemia.
If you have hypogammaglobulinemia, you may not need any treatment. However, if you get lots of infections, you may be offered treatment with immunoglobulin therapy given either into your vein or as an injection in your tummy. For more information on hypogammaglobulinemia click here.
Fatigue is a common symptom of lymphoma, and side-effect of its treatments. It is also a symptoms people tend to struggle with after treatment.
Remember that your body has been through a lot fighting the lymphoma and recovering from the treatments. Go easy on yourself and allow your body time to recover.
Ongoing fatigue however can impact your quality life and ability to get back to work, school or activities of daily living.
Fatigue should improve in the months after finishing treatment. However, for some people, fatigue can last several years, and some people may never return to their pre-lymphoma energy levels. If fatigue is an ongoing issue for you, speak with your GP about what support is available to you.
Also, for tips on managing fatigue and getting quality sleep, see the links below.
Peripheral neuropathy is caused by damage to the ends of your nerve cells that are outside of your brain and spinal cord. The most common places to experience peripheral neuropathy is in your fingers and toes, however it can extend up your arms and legs. It can also affect your genitals, bowels and bladder.
Nerve cells generally take longer to recover than other cells in our bodies, so peripheral neuropathy can take many months to improve.
The sooner you report symptoms and get treatment (or dose reduction of chemotherapy during treatment) the more likely your peripheral neuropathy is to improve. However, in some cases the peripheral neuropathy may be permanent.
You will need management strategies to decrease your risk of injuring yourself because of the neuropathy such as through burns or falls due to a change of sensation. You may also need medical intervention to improve the pain and discomfort you feel. for more information on peripheral neuropathy and how to manage it, see the link below.
Peripheral neuropathy – Lymphoma Australia
You may not need any scans after you finish treatment. Your haematologist or oncologist has other ways to monitor your progress and to check for any signs of your lymphoma returning.
Before ordering more scans such as PET or CT scans, they will weigh up the risks and benefits. Each time you have one of these tests you are exposed to a small dose of radiation. Over time, repeated scans can increase your risk of developing another cancer.
When your CVAD is removed will depend on:
- The type of CVAD you have.
- Ongoing supportive treatments you may need.
- How often you will need blood tests and whether these can be done without a CVAD.
- Length of waitlist to get into theatre to have it removed (if you have an implanted port-a-cath).
- Your personal preferences.
If you are eager to have your CVAD removed, talk to your treating haematologist or oncologist about when the best time would be.
Implanted port-a-caths need to be removed surgically so often take longer to be removed, depending on wait times for theatre. Other CVADs need a doctor’s order to be removed, so your nurses will not be able to remove it without the doctor’s order.
In some cases you may be able to have your PICC line or other non-implanted CVAD removed of the same day, after your last treatment.
You will need to continue to use barrier protection such as condoms or dental dams with lubricant for 7 days after you last have chemotherapy. After 7 days you do not need to use condoms or dental dams, but may need to still use other forms of contraceptive to avoid pregnancy.
Your libido (sex drive) may take time to come back as there are many things that can affect it. Fatigue, pain, nausea, anxiety and how you feel about changes to your body can all affect your libido. Additionally, some of your treatments may cause vaginal dryness or difficulty getting or keeping a strong erection. You may also have more difficulty reaching organsm. All these things can affect your libido.
If you have any on going problems such as those listed above, talk to your doctor. There is help available to improve these things. Also see our sex, sexuality and intimacy webpage by clicking here for more tips.
Having treatment for lymphoma can make getting pregnant or getting someone else pregnant more difficult. However, some people may still achieve a pregnancy naturally. If a natural pregnancy is not possible, there are other options available to help you get pregnant.
When is the safest time to plan a pregnancy?
You will have extra considerations before planning a pregnancy. Some factors that may influence when you can safely start planning a pregnancy include:
- The type of lymphoma you had/have.
- What type of treatments you’ve had.
- Any ongoing supportive or maintenance treatments you need.
- Side-effects from treatments you have had.
- The chance of your lymphoma relapsing and you needing more active treatment.
- Your physical, emotional and mental health overall.
- The method for getting pregnant.
Talk to your haematologist or oncologist about your desires for having a baby and ask their advice for when is a safe time to start trying. They can help advise you on when is the best time, and also refer you to a fertility clinic or for fertility counselling if needed.
For more information on fertility after treatment click the below link.
Many of our patients say they found comfort, and confidence to face what was ahead by learning about other people’s experience with lymphoma. If you would like to share your story, or read other’s stories click here or email enquiries@lymphoma.org.au.
There are many ways you can get involved to improve the lives of others living with lymphoma. Click here to learn about some of the ways you can get involved with Lymphoma Australia.
Summary
- Finishing treatment for lymphoma is a big deal, and you may experience mixed emotions for some time after your last treatment.
- You need a regular GP to provide ongoing support and follow-up care.
- You may still experience side-effects after treatment ends. Some may be ongoing side-effects, and some may start months or years after treatment ends. See the links above for how to manage side-effects.
- Ask your GP about a GP management plan, mental health plan and survivorship plan to help plan your health-related needs over the next year.
- Returning to work or school may take some extra planning. Use the tips above to help make the transition back.
- Fear of a relapse is common, but if it affects your quality of life and stops you planning a future, talk to your doctor, psychologist or our Lymphoma Care Nurses.
- A life-coach can help you set and achieve realistic goals.
- Report all new, or lasting symptoms to your GP and haematologist or oncologist.
- Let the people around you know you need so they can support you.